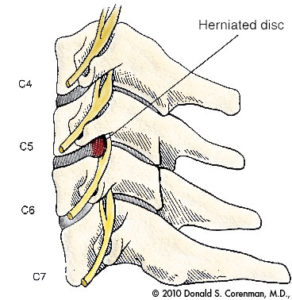
Cervical Disc Hernia: In order to understand what a cervical hernia is, we first will explain the structure of a cervical disc. It is a cartilaginous pad formed by a soft central part (nucleus pulposus) and another in the form of a fibrous ring that surrounds it. Its function is to absorb the loads to which the spine is subjected and cushion the movements that occur between two adjacent vertebrae.
Regarding the factors that influence the appearance of a cervical hernia we must differentiate between acute-soft disc herniation that usually occurs in young patients and whose cause is usually traumatic, and degenerative disc disease, in which the disc appears degenerated disc and dehydrated, and that is typical of cervical osteoarthritis.
In the acute hernia, the rest of the cervical spine is usually preserved, but in the degenerative, there is a decrease in the height of the disc (impingement) and a bulging (protrusion), in addition to the formation of bone spikes (osteophytes). The differentiating factor that exists between cervical hernia and lumbar hernia is that cervical hernia can cause spinal compression and the lumbar hernia cannot.
Symptoms
The symptoms are of three types: cervical pain, irradiated pain to the extremities and spinal compression. Cervical pain is located in the neck and can radiate to the head and shoulders. When a nerve root (radiculopathy) is compressed, pain radiates to the shoulder and upper limb. Depending on the root involved, pain may radiate to the shoulder and pectoral (C4-C5), reach the 1st finger (C5-C6), the 2nd and 3rd fingers (C6-C7) or the 4th and 5th fingers (C7-C8). In addition to the tingling sensation, there may be loss of strength in certain muscles and patients sometimes report that things fall out of their hands. Some improve raising the arm and placing the hand behind the head. Spinal compression causes a progressive loss of strength in all four limbs.
Diagnosis
The studies first cover the radiograph, which can show us degenerative changes, bone spikes, impingement, alteration of cervical dynamics or loss of normal curvature of the spine. In second place is the electromyogram (EMG), to know which root is more compromised or to differentiate a root compression from a peripheral nerve involvement such as carpal tunnel syndrome. And the definitive study is Nuclear Magnetic Resonance (NMR), which shows the state of the discs, if there is protrusion or hernia, if they are degenerated and dehydrated, compression of nerve roots, spinal deformity and most importantly, spinal compression.
Treatment
The diagnosis of a herniated disc is not necessarily synonymous with surgery. Generally, you have to start the first two weeks with anti-inflammatory treatment, application of cold or heat, modification of physical activity and sometimes immobilization with a collar. The third week we will start isometric and muscle strengthening exercises and from the fourth week, the rehabilitation phase begins. With this treatment, a satisfactory result can be expected in 70 to 80% of cases. But there are patients who persist with root pain after 6 weeks, have a neurological deficit with loss of muscle strength and sensitivity or clinical spinal compression. It is in these cases when surgical treatment must be considered.
You might also want to read:
How is cervical disc replacement surgery performed?
Benefits of cervical disc replacement surgery

